Live Event
Real solutions from experts who've moved the needle on burnout
Register NowTABLE OF CONTENTS
Radiology scheduling is highly complex, with teams scheduling providers across numerous specialties and locations. As a result, building the schedule is a task often reserved for physicians or administrators with deep knowledge of how their teams operate. Though this process is standard for many practices and healthcare organizations today, it often presents its own set of problems.
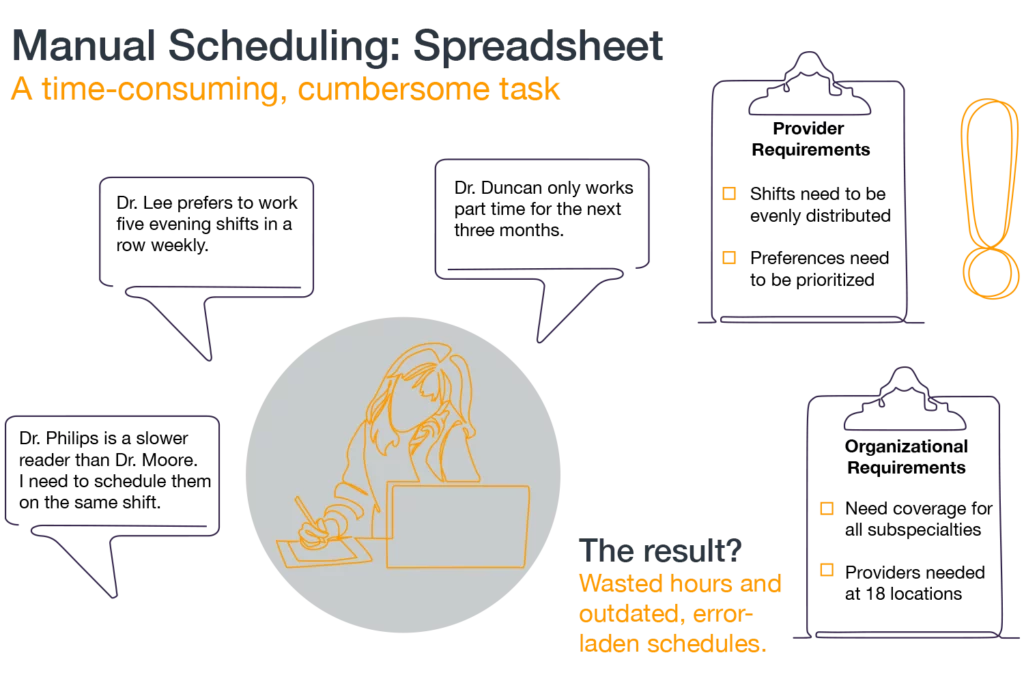
Creating shift schedules for radiologists is a major balancing act, with multiple scheduling variables that often compete against one another. Without leveraging the right tools to build schedules, radiology groups get stuck with a time-consuming, inefficient process that typically requires hours to create, edit, and distribute schedules. Let’s explore some key issues that contribute to the complexity of radiology scheduling.
Many diagnostic imaging exams and interventional procedures require specific subspecialty coverage. Radiologists are typically credentialed to work only one particular sub-specialty, with few able to provide cross-coverage care. The increasing sub-specialization of radiology, coupled with the growing shortage of radiologists,1 makes this all the more challenging.
Ensuring all shift types are covered without overutilizing certain providers is increasingly difficult. The consolidation of radiology practices and healthcare systems has forced many radiology groups to adjust their staffing models, which impacts imaging volume, hiring capabilities, workplace efficiency, patient care, and physician well-being.2
Radiologists and radiology technologists typically cover multiple locations, from imaging centers to hospitals. This makes the accuracy of existing manual schedules questionable, as it’s hard to determine who’s scheduled for what location and at what time. Add in the varying shift types at each individual location, and the equation becomes even more challenging. And because radiologists are a key component of the success of value-based care, it’s essential to staff locations accordingly.3
Radiology is quickly becoming one of the most challenging and expensive specialties for physician recruitment.4 The Association of American Medical Colleges estimates a shortfall of nearly 42,000 radiologists by 2033.6 As a result, it’s incredibly important to create schedules that minimize burnout and keep providers happy.
That means schedulers need to create schedules that factor in individual physician preferences, allow adequate time between long or taxing shifts, and ensure shifts are evenly distributed among providers. However, given the large number of scheduling variables, some radiology groups struggle to make provider satisfaction and well-being a priority when building schedules.
Like most industries, each team (and each provider) works at different speeds to manage patient care and administrative duties. Some radiologists can read 11 films in an hour, while others can only read eight. A scheduler must know in advance to account for various productivity levels, much like they must account for different provider preferences. If they don’t know about varying productivity levels in advance, they may have to go back and make further edits to the schedule, increasing the time spent on this already cumbersome task.
Despite the existing complexities associated with radiology scheduling, some radiology groups still build shift schedules manually—by hand or spreadsheet—instead of using automated radiology scheduling software.5 Unfortunately, manual scheduling often leaves gaps in coverage, requires cumbersome manual edits, and fails to maximize existing physician and administrative resources. The downstream consequences of a suboptimal schedule can contribute to physician burnout, whether because shifts aren’t distributed equally or because oversights lead to frustrating operational hiccups. Schedules built manually also tend to be written by hand or typed into a computer, meaning a scheduler has to individually send the schedule—and any edits thereafter—to each person who needs to see it.
In contrast, optimized radiology scheduling software is much more efficient and cost-effective. It grants physicians more autonomy over their work preferences, flexibly schedules providers across various locations, maximizes resources, and saves physicians and administrative staff hours of their time by automating the schedule-building process. Plus, with an automated schedule builder, any edits made after the fact can be updated in real time, and providers accessing the schedule will be notified of all relevant changes when they occur. These schedules are also accessible on desktop and mobile apps, meaning no provider is left behind when the schedule is published.
Greenville, North Carolina-based Eastern Radiologists, LLC, was unsatisfied with their manual schedule-building process. The subspecialty radiology practice supports 18 locations, including six imaging centers and 12 hospitals, and manages a total of 61 provider schedules. To build these complex schedules, they relied on an Excel spreadsheet. It was an imperfect process, to say the least.
Eastern Radiologists had to build schedules that accounted for various organizational requirements, coverage for all specialties, fluctuating patient demand, and provider preferences. In particular, they struggled to schedule a balanced number of “slow readers” (providers who are newer or tend to work slower than others) and faster readers. They faced other problems as well:
After switching to PerfectServe’s Lightning Bolt Scheduling, Eastern Radiologists implemented 385 unique schedule rules as part of a new automated scheduling process. This included, for example, a rule that only one slower reader could be scheduled at each location per shift. The automated process can also easily handle time-off requests, equitable shift distribution, and individual provider schedule preferences, such as preferred work days or the maximum number of consecutive shifts they’d like to work. This leads to schedules that better balance the needs of the organization with the needs (and wants) of providers.
Additionally, Eastern Radiologists are now able to download and analyze shift data to ensure equal distribution of work among all of their providers, including the ability to see who swapped shifts, who picked up shifts, and who may have dropped shifts or taken vacation time. Lightning Bolt is able to generate this and many other reports to improve resource allocation and ensure workload equity. All of their implemented rules are now automatically considered to create the best possible schedule that meets organizational needs, accounts for provider preferences, and maximizes resources. You can watch an on-demand webinar featuring their Lightning Bolt experience here.
Interested in learning more about optimized schedules? Contact us today to learn how you can ditch the manual work in favor of Lightning Bolt’s automated scheduling solution.
Sources
1,6 Physician Specialty Shortage – Including Radiologists – Continues to Climb, Diagnostic Imaging, Whitney J. Palmer: diagnosticimaging.com/view/physician-specialty-shortage-including-radiologists-continues-to-climb
2 Around-the-Clock Radiology Coverage: Challenges and Opportunities, Applied Radiology: https://appliedradiology.com/Articles/around-the-clock-radiology-coverage-challenges-and-opportunities
3 Radiology in the era of value-based healthcare: a multi-society expert statement from the ACR, CAR, ESR, IS3R, RANZCR, and RSNA, Insights Imaging: https://insightsimaging.springeropen.com/articles/10.1186/s13244-020-00941-z
4 Physician Recruitment: The Cost to Hire and Return on Investment, Jackson Physician Search: jacksonphysiciansearch.com/physician-recruitment-the-cost-to-hire-and-return-on-investment/
5 In the Flow: Part 2 — Equitable Scheduling Prevents Burnout, Delivers Better Patient Care, Radiology Today—Vol. 19 (No. 3), Page 24, 2018: radiologytoday.net/archive/rt0318p24.shtml