Live Session
A Roadmap for Change Management Projects
Register NowTABLE OF CONTENTS

Staffing shortages, physician burnout, elevated turnover rates, and declining provider satisfaction levels are challenges that have been present to varying degrees in healthcare for a long time. Would it surprise you to learn that ineffective provider scheduling is often a substantial contributing factor for each of these challenges? Too often, schedules are imbalanced and flawed, leading to negative outcomes like decreased productivity, increased time to locate and connect with the correct provider, inadequate resource utilization, patient leakage, and revenue loss. And because outdated scheduling processes that rely on pencil & paper or Excel spreadsheets have never offered much insight about how schedules can be meaningfully improved, decision makers may not be fully aware of more advanced tools that exist to drive operational efficiency. By implementing an optimized, rule-based scheduling solution across all departments at your organization, operations leaders can more clearly see resourcing gaps and opportunities to improve organizational metrics. More specific benefits include:

According to the AMA, the cost of physician burnout can range from $500,000 to more than $1 million per provider when they leave or reduce their clinical hours. This estimate accounts for recruitment, bonuses, lost billings, and onboarding costs1 . Staff retention is a critical component of a healthy enterprise, and scheduling software can be an effective tool in your burnout-prevention toolbox. Automated scheduling solutions can build more equitable schedules for each department, make them available digitally, and keep track of individual provider preferences and requests to automatically apply them to the schedule. This allows for:
An Excel worksheet is a slow and frustrating medium for building schedules, so investing in an automated solution can yield a wide range of downstream benefits. Tech-enabled solutions can combat the complexities of burnout and low provider satisfaction levels by building schedules that distribute work evenly while considering the needs of both the providers and the organization.

Research suggests that up to 40% of communication time is spent searching for contact information or attempting, but failing, to reach the correct provider.2 Slower, more fragmented communication delays patient care and leads to time-wasting activities for care team members like:
Giving care team members access to a real-time on-call schedule and integrating it with other systems, like the operator console or a clinical communication platform, can mitigate these communication obstacles.

Many organizations haven’t fully realized the power of scheduling as it relates to resource utilization. There are three distinct areas where schedules make an impact:
These resources are often managed manually via Excel or using disparate solutions, which takes time and leaves significant room for error. What’s more, data-driven insights can’t be easily extracted from manual scheduling workflows, meaning operations leaders often can’t see which departments may be under or overstaffed or if operating rooms are being utilized to their full capacity. Partnering with a scheduling provider that can balance people, resources, equipment, rooms, and patient demand with one solution that spans the entire organization can turn frustration into opportunity.
Operations leaders can use the checklists below to thoroughly evaluate the features and benefits of advanced scheduling technology:
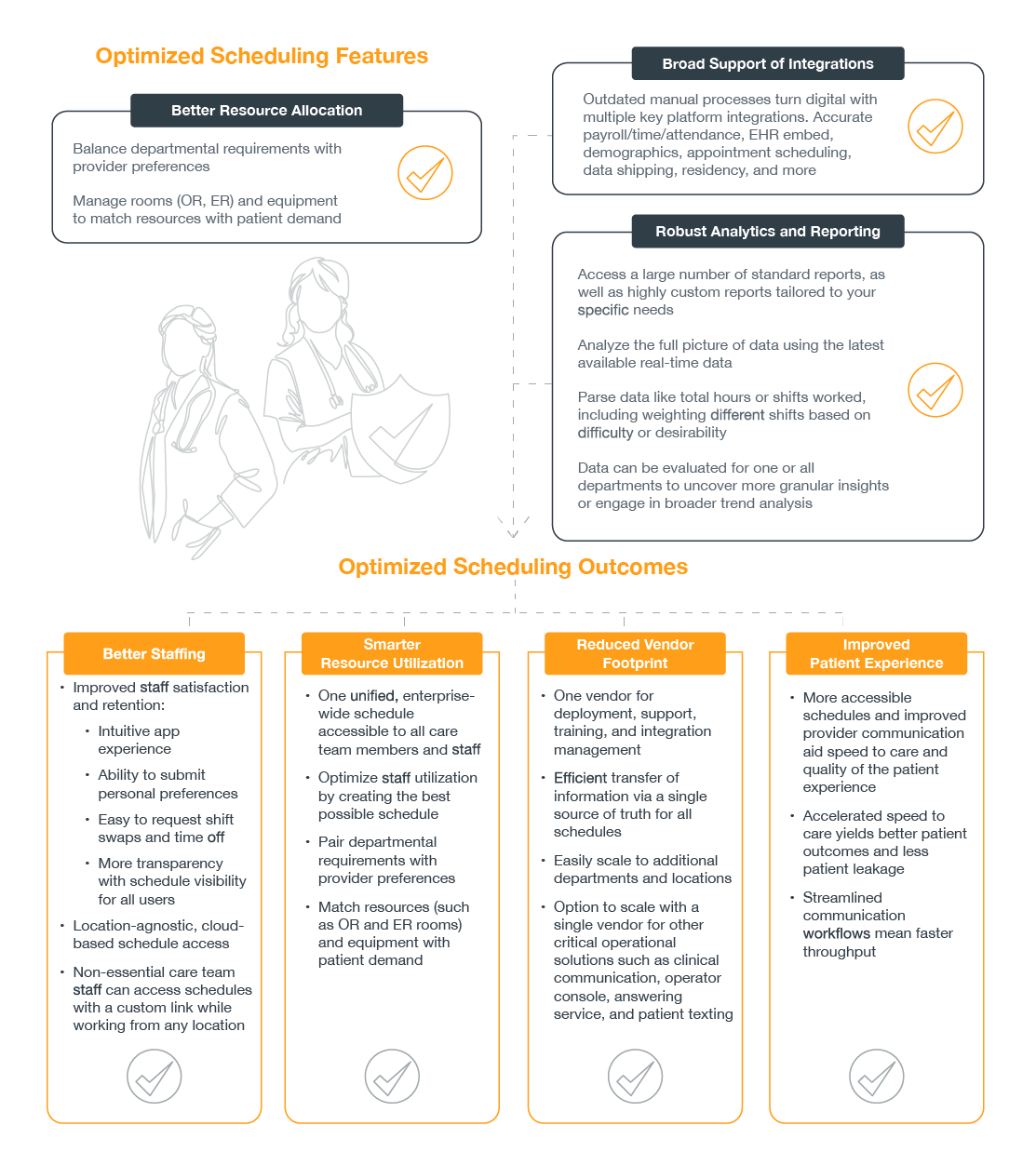
Rule-based scheduling software can help operations leaders improve a myriad of workflow issues that impact operational efficiency. Decision making instantly becomes more informed with data that can be parsed all the way from the department level to the health system level. Automated scheduling can help operations leaders achieve a wide variety of organizational goals:


Locate and Connect
Nurse Gilda needs to contact the on-call hospitalist regarding the status of one of her patients. With no scheduling solution in place, she has to travel to the nurse’s station, open a binder, locate the schedule for that department, and look at the current hospitalist schedule. Of course, Nurse Gilda hopes there haven’t been any changes since the schedule was printed.
Finding that Dr. Johnson is the hospitalist on call and is caring for her patient, she picks up the phone to call him. She finds that Dr. Johnson is in surgery and is unable to respond at this time. Nurse Gilda now has to return to the schedule to find the contact information for the next on-call physician. If the second physician is unavailable, the process will repeat itself until Nurse Gilda can locate a hospitalist who can speak with her about her patient.
Problem: Providers and care team staff experience frustration when trying to locate the appropriate on-call provider—time that could be better spent caring for patients.
How do optimized schedules solve this problem?
A digitized, widely accessible schedule allows providers and other care team members to see the schedule from anywhere. When integrated with a clinical communications platform, any user can simply click to connect to the appropriate provider, and the platform will automatically contact them according to their contact preferences. If that provider doesn’t answer, the message can be automatically routed to the next on-call provider depending on the nature of the message.
Results:
This workflow takes the time to connect down to seconds—dramatically enhancing speed to care and eliminating clinician frustration.

Easier Workflows, Improved Results
Sue has an appointment with her primary care provider, Dr. Smith. She presents with a cough, shortness of breath, and fatigue. Dr. Smith examines her and recommends that Sue’s daughter take her to the ED for breathing treatments, an X-ray, and some additional testing.
Dr. Smith calls the hospital transfer center to give a report about Sue’s condition to the ED physician on call. The transfer center operator is able to quickly search in the operator console for the “ED On-Call.” The system automatically shows that Dr. Taylor is the oncall doctor for the ED, so the operator is able to send a secure message from the operator console to ask if Dr. Taylor is available for report. The operator is then able to connect Dr. Smith and Dr. Taylor in a timely manner.
Problem: Without an automated and integrated scheduling solution, the operator may have had to consult an Excel schedule, which may or may not have been completely accurate. If the schedule were incorrect, the operator would have to circle back to try and track down the right provider, and Dr. Smith would simply be left waiting. This could lead Dr. Smith to choose another, more efficient facility in the future, and therefore poses a potential loss of revenue for the facility with dated scheduling practices.
How do optimized schedules solve this problem?
This improved communication workflow happens thanks to:
Results:
The seamless process leads to a number of positive results:
Resource Utilization
Milo, a program manager and scheduler, is using optimized scheduling for his providers across multiple departments. By looking into the data and analytics provided, he notices that Dr. Rhoades worked fewer shifts than his fellow doctors over the past two months. Upon further research, Milo finds that patient demand has been lower during that time, which means not as many providers have been needed for on-call shifts. The clinic, however, has been slightly under-staffed. Because Milo can see this data, it’s easy for him to move Dr. Rhoades off of the call schedule and assign him three extra clinic shifts for the next month.
Problem: When resources are underutilized and providers are overworked, it can elevate provider frustration and stretch already tenuous budgets. When patient demand outstrips available providers, it can lead to burnout, wasted resources, lost productivity, patient dissatisfaction, and slower treatment times.
How does optimized schedules solve this problem?
A single source of truth for schedules lets users compare areas of the hospital to see which departments are understaffed or overstaffed each day. For operations leaders and schedulers, this gives detailed insight into where resources are strained and where they could be better allocated.
Results:
Departments can easily see who’s scheduled to work at the clinic versus on call, and patient demand can be met by ensuring the right number of providers are scheduled. This insight helps the organization avoid wasted resources, loss of productivity, and poor care delivery.

With Lightning Bolt, decision makers get a more detailed look at how scheduling is helping—or hurting—strategic growth. Rule-based technology like Lightning Bolt can then be bolstered to optimize schedules, increase resource utilization, protect patient leakage, improve ROI, and strengthen speed to care. Through key integrations, wellness surveys, automated scheduling, and detailed analytics, Lightning Bolt is a powerful tool to support enterprise-wide growth and management goals by boosting provider satisfaction, increasing resource utilization, preventing patient leakage, and improving communication workflows throughout the entire health system.