TABLE OF CONTENTS
Three Essential Considerations for an Enterprise Scheduling Solution
When seeking a scheduling solution, large organizations should begin with three essential questions:
- Will a single solution support the needs of every department, or will additional scheduling tools need to be purchased for each department’s unique needs?
- Will this system improve provider satisfaction or create more frustration?
- Will it improve key performance metrics for the organization?
Accurate, easy-to-access schedules are critical to effective communication. Each year, breakdowns in communication cost hospitals more than $11.2B, and inaccurate schedules are frequently part of the problem.1 For healthcare provider organizations, centralized scheduling can have a significant positive impact on sentinel events, time to treatment, burnout, length of stay, and patient experience. In this guide, we’ll outline how to evaluate enterprise scheduling systems and key use cases to consider when choosing a solution.
Meeting the Needs of the Enterprise
Some hospitals and health systems deploy “enterprise” scheduling systems only to discover over time that they don’t meet the unique needs of every department. Because additional systems then need to be purchased, this leads to an increased total cost of ownership for the organization. It also limits access to enterprise-wide analytics because it can be technically challenging to centralize disparate scheduling systems.
Organizations seeking a single provider scheduling solution to support dozens of departments and locations must evaluate whether the system can create schedules that accommodate:
- Organizational needs
- Departmental needs
- Individual provider preferences
If a scheduling tool is unable to accommodate any one specialty rule, it won’t deliver the right results. Yet, some organizations attempt to deploy a one-size-fits-all scheduling system with little flexibility across every department, which ultimately fails to meet the organization’s needs.
Every Specialty Has Unique Scheduling Needs
For example, a hospitalist department alone requires hundreds of scheduling rules. To name a few:
- All full-time equivalent (FTE) providers must work a set number of shifts each month/year.
- Providers are scheduled a minimum number of shifts in a row for continuity of care.
- Providers only work a maximum number of shifts in a row to prevent burnout.
The variance of scheduling requirements across departments can be challenging. A surgical group, for example, has different scheduling needs than the hospitalist group or
the OR. As you begin the search for a scheduling solution, document how schedules are created across departments and locations and what factors impact each schedule.
Once you have insight into the needs of every department and location, choose a solution that can accommodate all needs throughout your organization. The ideal solution will offer the flexibility to meet a variety of scheduling needs within one central platform. To verify a potential solution has the capabilities you need, don’t just ask the vendor. Look for existing users who will share their experience with the solution.
Improve Provider Satisfaction, Reduce Burnout
Many scheduling tools tout the ability to improve provider satisfaction and decrease burnout. Let’s explore some tangible ways scheduling can impact provider satisfaction, both positively and negatively:
- Ease of use when requesting time off
- Ability to quickly swap shifts with colleagues
- Ease of looking up other providers and on-call providers
- Capability to view schedules from any device
- Overscheduling, or the inequitable distribution of certain shifts including call
- Accommodation of provider scheduling preferences, such as shift type (e.g. back-to-back shifts/call, preferred days and times)
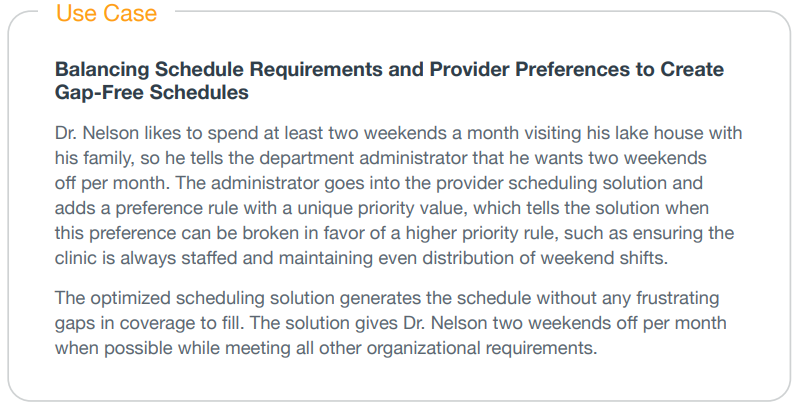
To improve provider satisfaction, it’s important that the solution both simplifies scheduling workflows and incorporates provider preferences. If the solution can’t easily accommodate provider preferences, it delegates an extremely challenging— at times even impossible—manual task to the scheduler.
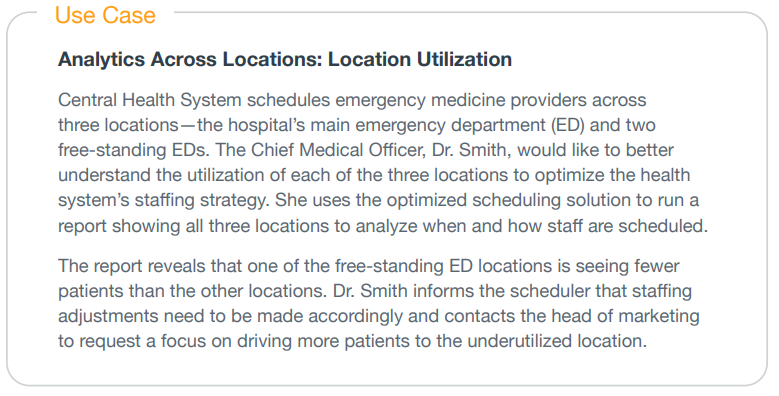
Key Metrics You Need
A scheduling solution can play a powerful role in improving key metrics for healthcare organizations. When you deploy an enterprise-wide scheduling solution with advanced workforce analytics, your organization can begin tracking progress across a number of metrics, including:
- Location utilization and staffing levels.
- Service utilization across departments and locations.
- Assignment coverage across care services, locations, and departments.
- Gap analysis between patient demand and provider supply.
- Reports on time-off requests and approvals.
- Time tracking, shift tally, and other shift distribution reports.
Insights into these metrics can reduce costs, minimize time spent creating and managing schedules, cut labor costs, improve patient and provider satisfaction, and decrease time to treatment.
Advanced Use Cases
Beyond meeting the basic needs of generating simple schedules and allowing you to look up who is on shift or call, let’s explore some advanced capabilities you can only get from an optimized enterprise scheduling solution.
Evaluating Solutions
When choosing an enterprise-wide scheduling solution, consider asking vendors the following questions.
Product Functionality
How complete/gap-free are the schedules generated by your system?
Many scheduling platforms on the market use a heuristic method to generate schedules—meaning they often sacrifice accuracy and completeness for speed. Unfortunately, this shortcut often generates schedules filled with gaps in coverage that administrators then have to fill in manually, reducing the time savings associated with the scheduling tool.
Does the system have different levels of functionality to meet different department needs?
Not all departments have schedules that require advanced rule-based scheduling. Ensure that the vendor you choose offers basic scheduling for groups that only need limited functionality and more advanced options for departments with complex schedules—instead of a costly one-size-fits-all solution.
Mobility
Does the platform offer a native mobile application?
One of the most valuable features of a digital scheduling solution is real- time access to schedules across your organization from any mobile device. Ask vendors detailed questions about the mobile app’s functionality. Does it offer a similar level of functionality to the desktop version? Can schedulers make edits to the schedule from their mobile device? Can providers swap shifts and request time off from anywhere?
Speed to Value
How quickly will your organization reap the benefits of your new scheduling solution?
Although most advanced scheduling solutions can take anywhere from 9-12 weeks to fully implement, your team should begin seeing some of the benefits within the first
two weeks of implementation.
Implementation
Is the implementation model one-size-fits-all?
The vendor you choose should be willing to prioritize your organization’s biggest needs first and partner with your team to build a rollout model with your best interests in mind. For example, if inaccurate call schedules are a big pain point for your care teams, then rolling out the call schedule functionality should be a priority by week two of implementation.
What integrations are available?
Integrations are key to ensuring your scheduling solution works seamlessly across your network of systems and data to add value to other clinical workflows. Below are important integrations and how they work with an optimized scheduling solution.
- Communication and Collaboration Solution: Ensure communication always reaches the right provider at the right time by syncing real-time shift and on-call schedules with your communication platform.
- HR System: Keep contact information up to date in your scheduling solution by pulling in the latest provider information.
- Payroll, Time, and Attendance: Automatically share time tracking data with payroll and other systems to eliminate manual data entry.
- Business Intelligence System: If your organization leverages a data lake or business intelligence system, ensure your scheduling solution seamlessly delivers information to the system to easily interpret data.
- Electronic Health Record (EHR): Integrating your scheduling solution with your EHR allows care team members to see real-time physician availability from within the EHR.
Final Considerations
Don’t underestimate the value of finding the right scheduling solution. Optimized scheduling supports provider satisfaction while adding substantial value to the hospital’s bottom line in vendor consolidation, efficient resource allocation, improved staffing capabilities, enhanced communication workflows, and administrative time savings.
Getting Started
To learn more or reserve a demo with an innovative technology partner that has more than 20 years of experience solving clinical communication and provider scheduling workflows, please contact us:
866.844.5484
sales@perfectserve.com
Sources 

- The Imprivata Report on the Economic Impact of Inefficient Communications in Healthcare, Ponemon Institute, Jun. 2014: ponemon.org/local/upload/file/2014%20Imprivata%20Report%20FINAL%203(1).pdf
- Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study, Springer Nature, Maryam S. Hamidi et al., BMC Health Services Research-18(1)-851, Nov. 27, 2018: doi.org/10.1186/s12913-018-3663-z
- At Stanford, physician burnout costs at least $7.75 million a year, American Medical Association, Sara Berg, American Medical Association, Nov. 17, 2017: ama-assn.org/practice-management/physician- health/stanford-physician-burnout-costs-least-775-million-year
- Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide, Medscape, Jan. 15, 2020: medscape.com/slideshow/2020-lifestyle-burnout-6012460 – 5
- Physician Turnover at All-Time High, Becker’s Healthcare, Becker’s Hospital Review: beckershospitalreview.com/hospital-physician-relationships/physician-turnover-at-all-time-high.html
- Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide, Medscape, Jan. 15, 2020: medscape.com/slideshow/2020-lifestyle-burnout-6012460#5