Live Session
A Roadmap for Change Management Projects
Register NowTABLE OF CONTENTS

Schedules could be considered the engine of a healthcare organization because they dictate the who, what, when, where, and how of care delivery. But because they’re so intertwined with each shift a provider works, you have to think beyond the where, the when, and the who—the quality of the schedules is also critical.
If schedules overwork and overburden providers, the organization will likely experience provider stress, increased burnout, and higher turnover, not to mention the downstream impacts of delayed patient care.
Turnover is costly. Data suggests that turnover costs nearly $1.2 million per provider, and the average annual start-up cost for a new doctor is $211,000.1
The good news? Schedules created to optimize workflows, accommodate provider preferences, and maximize productivity can improve provider satisfaction levels to boost employee retention. Here’s how.
Traditionally, providers have limited ability to influence their schedules. Outdated manual scheduling workflows don’t leave much room to accommodate their preferences and aren’t exactly flexible when supply and demand don’t match.
That means providers have to deal with the consequences of ineffective schedules. Excessive workloads and long working hours are some of the most commonly cited reasons for provider frustration2, increasing the risk of burnout and eventual turnover.
Here are just a few examples of how this frustration might play out:
In both scenarios, suboptimal scheduling practices are a drag on physician job satisfaction. That’s not acceptable.
With optimized scheduling in place, things are different.
The elevated patient census for this month means there are two more anesthesiologists working this shift than normal. Let’s say you’re one of them, but you know the schedule will account for this because it balances shifts across the entire year. For the next two months, you won’t be pulled in for extra shifts.
Your patient’s labs have just been received, and you need to consult another physician before making the final arrangements for your patient’s discharge plans. You check the schedule to see who to call and quickly see that Dr. Clark is working. You call her, and she picks up after just one ring.
You entered a preference not to work first call on Fridays when possible, and you’ve only had to do this once when your coworker took time off. You submitted a time-off request next month for that much-needed family getaway, and thanks to the optimized schedule, your request was granted.
What’s more, your partner asked for your schedule to plan a date night next week. You sent them a public link to check your schedule, and now you’ve got dinner and a movie planned for next week.
All of these benefits are easily achievable for all providers with an optimized scheduling workflow in place. Better schedules:
Heavy workloads and unfair schedules are just a few pieces of the employee turnover puzzle. Schedules that aren’t optimized for what makes up a shift—patient appointments, calls, administrative duties—can make providers feel burned out from rushing through their work day.
Let’s look at an example of how productivity can be impeded by inefficient scheduling:
This doesn’t have to be the norm in healthcare. What would happen if automated scheduling could ensure non-clinical time for providers and track educational requirements for residents?
Advanced scheduling can balance provider workload and ensure shifts are optimized to leave room for important administrative duties, patient care, academic time, and more. This has a few downstream effects, all of which can reduce employee turnover by:
Ochsner Health’s anesthesiology department handles more than 22,600 cases each year. Their team of 60 anesthesiologists manages a range of pre- and post-operative care, pain therapy, diagnostic services, and more.
Before optimized scheduling, schedulers spent 60 to 75 hours a month manually creating and publishing schedules with an Excel spreadsheet. The schedule managed both anesthesiologists and the entire anesthesia team, but there was no standard process for time-off requests, schedule changes, and other scheduling workflows.
Even when the schedule was finished, a number of edits were often needed. There was also no centralized place to access shift or call schedules, meaning care team members could be accessing outdated schedules without knowing it.
After implementing optimized scheduling, providers were able to submit requests and preferences for particular shifts. Transparent reporting provides more flexibility and predictability for matching patient demand with provider supply, and case assignments are now used to inform payroll, ensuring accurate and timely compensation.
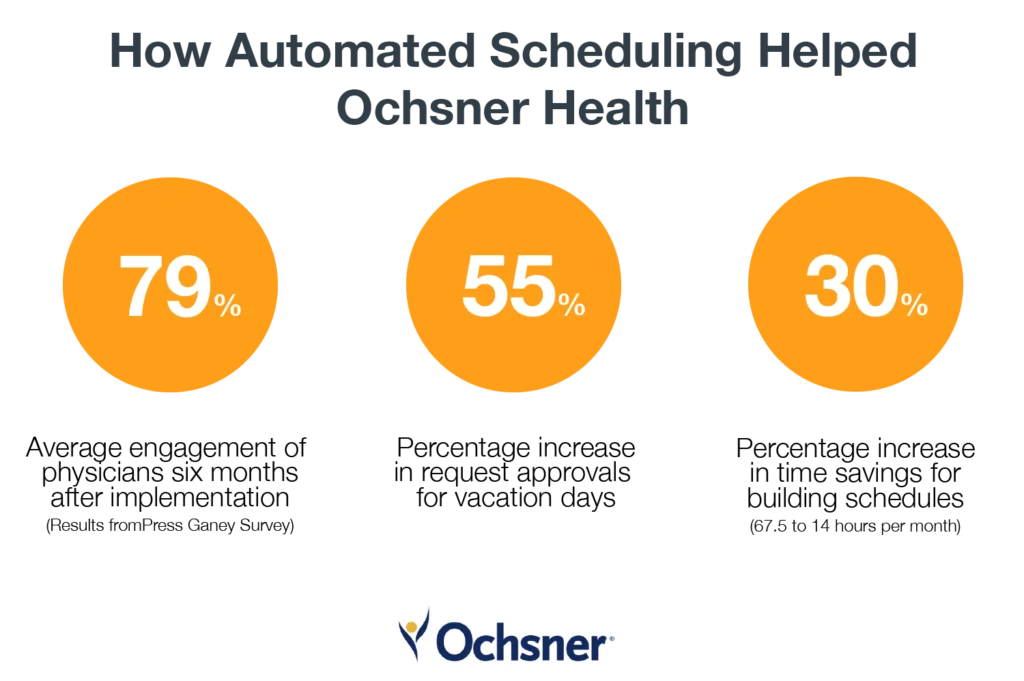
To learn more about Ochsner Health’s Lightning Bolt Scheduling outcomes—including an added benefit of $600k per year in savings—read the case study here.
Schedules are a critical component of a high-functioning health system. For just one piece of evidence, talk to any healthcare professional who served at the peak of the COVID-19 pandemic. Many of them experienced a total loss of autonomy—they had no control over the spread of the virus, and they had little to no control over the makeup of their day-to-day schedule as the pandemic unfolded. This degree of uncertainty is (thankfully) not always present in healthcare, but it’s a reminder that physicians and other care team members cannot perform at the highest level indefinitely with unbalanced and unpredictable schedules.
Optimizing schedules can reduce burnout, increase provider satisfaction, and boost productivity to support employee retention. If you’re ready to see how optimized scheduling can reduce your employee turnover, reach out to us today.
Sources: